Today’s Health Connector Board meeting focused on Health Connector accomplishments so far in FY 11, and Affordable Care Act Implementation progress in Massachusetts (materials).
The Board Chair, Jay Gonzalez, began by updating the board that the Governor signed the FY 12 budget on Monday, and he thinks it will positively change the way government does business. Included in the budget is sufficient funding to sustain subsidies for small businesses and to pay for the Commonwealth Bridge program for the year, pending a decision in the Finch case, which seeks re-integration of legal immigrants into Commonwealth Care. As part of Chapter 288 signed last year, the Connector Board was scheduled to add an insurance broker to the Board, but has not done so yet. Gonzalez gave his appreciation to Terry Dougherty, Director of MassHealth, as this was Dougherty’s last meeting.
Glen Shor, Executive Director of the Health Connector, then provided a brief update in Connector enrollment, which is about 1000 members down in June for both Commonwealth Care and Commonwealth Choice. There are now roughly 159,000 individuals enrolled in Commonwealth Care, and 38,000 individuals enrolled in Commonwealth Choice. The CommCare open enrollment period closed as of July 8th, during which 6.8% of existing members switched plans. Shor mentioned that the Connector website experienced some difficulties during this period due to increased volume, but the issue has since been resolved.
The Connector staff then reviewed the accomplishments for fiscal year 2011, and looked ahead towards the challenges of implementing national reform in Massachusetts. Just click for the rest of the story.
Bob Nevins, Chief Operating Officer of the Health Connector, provided an update of FY11 Plan of Operations Results. The plan of operations includes Health Connector goals in four areas: Program (Commonwealth Care and Commonwealth Choice), Policy, Administrative/Organizational, and National Health Care Reform. A list of key accomplishments:
- FY 12 Commonwealth Care achieved savings, where 4 out of 5 health plans had flat or reduced rates compared to FY 11 levels, resulting in $80 million in savings while preserving eligibility and benefits. In addition, greater than 1/3 of CommCare enrollees are now in narrower network plans with 19% lower costs for coverage. Nevins commented that he is pleased with these limited network results, but also recognizes these networks are experiments and the Connector will follow them closely.
- Sharp growth in Commonwealth Choice membership, where overall growth exceeds 9,000 members, or a 31% increase in enrollment. The Wellness program has launched for Business Express members, but it is too early to report on progress. There has also been fee reductions for small businesses and carriers.
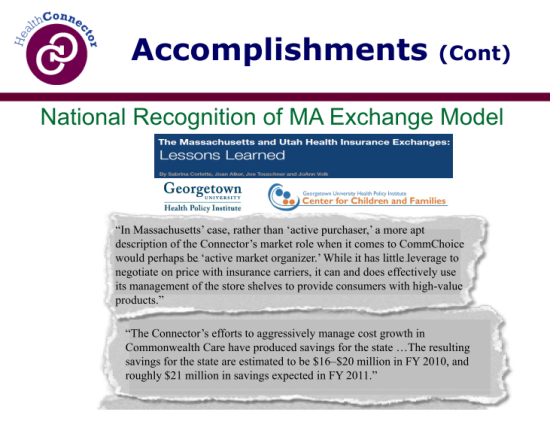
- Early implementation of national health reform has been successful, as Massachusetts has gained secure funding for planning and an early innovation 2-year grant ($35.6 million). The BCBSMA Foundation has developed a “Lessons Learned” report and Toolkit about MA Health Care Reform, which serves as a great tool for consumers and other interested parties, according to Nancy Turnbull. In addition, Massachusetts has served as a national model for insurance exchange.
- Improved student health procurement, promoting competition between carriers and adding prescription coverage and enhanced benefits to student health plans.
- Organizational excellence and innovation, in terms of member satisfaction, refreshed website homepage and shopping screens, and balanced administrative budget with lower state funding.
Nevins reported that of the 49 key strategies across the 4 planning categories, 40 (82%) have been completed, 4 are still in progress, and 5 have been deferred. Nevins said that when the Board set this year’s goals, they knew the goals were a stretch and the deferred goals should not be seen as a failure. Many were simply a result of lack of time or deferred in light of ACA implementation. Shor also pointed out that during the year, new opportunities and responsibilities arose that the Connector addressed, such as the National Health Reform Innovator’s grant.
Next, Stephanie Chrobak and Kaitlyn Kenney presented the National Health Care Reform Planning update. They began with the guiding principles of the Subsidized Insurance Workgroup, which was formed to assess the options available for providing subsidizing coverage in accord with national health reform. Chrobak said that they are at the very beginning of their timeline, which includes key federal dates to meet grant and planning deadlines. The timeline divides planning into three phases by year, 2011: the Assessment Phase, 2012: the Design Phase, and 2013: the Implementation Phase, with the goal of being ready to go live with the new model in 2014. The board stressed how planning needs to be done early in order to gain the appropriate waivers in time for 2014, and in light of the next CMS waiver expected to expire at the end of 2013.
So far, in 2011, the group has identified outstanding policy questions, guiding principles, potential options/approaches, and hired consultants to work on a strategic plan. Still to be accomplished in 2011 is soliciting feedback on policy options and evaluating components from leadership and the Health Connector Board, sharing the options with stakeholders, conducting comprehensive analysis of each model, performing a gap analysis, identifying the recommended approach for the delivery of subsidized insurance, and presenting the assessment to federal government.
Celia Wcislo questioned how the national debt ceiling debate could affect health reform in MA now and in the future, as a good chunk of money we use to subsidize individuals is provided through a federal waiver. This is a very uncertain area, but would seriously impact the ability of Massachusetts to subsidize health care, and federal issues will be taken into consideration while modeling for ACA implementation, according to Kenney. Wcislo also stressed the need for smooth transitions between Medicaid and other insurance options.
Some key concepts in thinking about ACA implementation in Massachusetts:
- Medicaid expansion: ACA mandates adults <133% FPL will be covered under Medicaid.
- Basic Health Plan Option (BHP): ACA provides state the option of establishing a basic health plan option, with at least the essential benefits package. Instead of individuals receiving tax credits to subsidize their coverage, the federal government will provide the state with 95% of the premium and cost sharing tax credit that would be given to the individual and the state will subsidize insurance. The hope is that if we choose to establish a basic health plan option, the state can negotiate it such that individuals will be better off than receiving tax credits in the exchange.
- Tax Credits: ACA will provide advanceable tax credits to eligible individuals with income from 133-400% FPL to purchase coverage in the exchange. Tax credits will be given on a sliding scale based on income, with individuals required to spend a certain percentage of income on health insurance.
- Essential Health Benefits (EHBs): ACA requires all plans offered to through the exchange to contain this package of benefits, which has yet to be developed by HHS. This requirement is similar to Minimum Creditable Coverage in the Health Connector.
The workgroup has developed 4 broad options for Massachusetts to subsidize coverage under national health reform (see our earlier post for some more details):
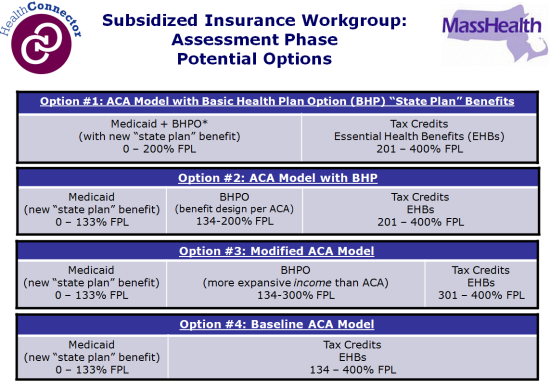
Each of these options will be assessed and evaluated based on what they will look like for given consumers. Dolores Mitchell asked how much of Massachusetts’ health exchange we will need to change in order to accommodate the ACA. Kaitlyn Kenney explained that this completely depends based on which option we choose, and we are in the process of weighing these options given the current population in Massachusetts.
Option 3 above is not expressly permitted by the ACA, as ACA permits states to establish the Basic Health Plan only for individuals with income up to 200% of FPL. However, this option is more akin to the way Commonwealth Care works in Massachusetts now, and conversations with federal officials have signaled that flexibility in state exchanges is encouraged, so this may be a viable option for the Commonwealth.
Terry Dougherty responded to a question made by Louis Malzone regarding Option 4, and commented that this would be the only option that would not require obtaining new Medicaid waivers.
Options will be evaluated based on several criteria, including federal and state finances, plan benefit design, stakeholder impact, and governance options.
The consultants at Manatt Health Solutions and Mercer are in the process of completing a baseline analysis, after which the subsidized insurance workgroup will review the analysis, assess the options and review open questions by stakeholders. Manatt/Mercer will develop quarterly progress reports that will culminate in a strategic plan. Jay Gonzalez stressed the importance of stakeholder involvement going forward in our planning, as many parties are committed to the goal of successful health care reform.
Kenney provided an update on the grant cycle. The Connector is recommending that they seek a No Cost Extension of the Planning Grant to December 31, 2011, which will give the vendor more time to complete research and analytics and address issues and questions that come up in the development of a strategic plan.
Lastly, states can apply for an Establishment Grant before December 31, 2011. Massachusetts will apply for Level II funding that lasts through 2014 and is a cooperative agreement, allowing the terms of the grant to be modified over time. There is no ceiling for this grant.
At the close of the meeting, Turnbull asked Kenney if the proposed regulations for exchanges yielded any surprises. Kenney says the no cost extension will be important for considering these regulations, and she will look more closely to discover key takeaways relative to the Health Connector.
-Amelia Russo

What if states does not implement the basic health program?